![]()
![]() #rideforgarai
#rideforgarai
Longest Ride Challenge 2018
I was proud to sign up and commit to this challenge. This was despite my current longest ever ride (the ride to better, set 12 months ago) being an intentional once-in-a-lifetime 100.1 mile effort! This was at the West Coast Classic – action pics below!

I hoped to join Idai Makaya to ride with him on a section of his Longest Ride Challenge 2018 – a Lejog-Jogle (Lands End to John O’ Groats to Lands End) Guinness World Record attempt on his ElliptiGO cycle. My plan was to meet up with local fellow ElliptiGO rider Andy Nuttall, ride to Warrington (25+ miles) to join Idai and ride with him until Lancaster (50 miles) on that section of his ride and, finally, to ride a slightly indirect route back home (25 + miles) with Andy!
Well, that was the plan! However, now my circumstances dictate that I will be unable to complete the Longest Ride Challenge 2018 in its intended format. I still wish to support the #rideforgarai and Longest Ride Challenge 2018 initiative so, my new plan is to promote them through this post in my blog, in the hope that some of my running and cycling friends may be inspired to take up the challenge during the year.
In order to generate interest in this post, I will now explain why I can no longer fulfill my original plan, nor better my previous longest ride. The post will also explain why I have been absent from Strava and generally out of circulation for a few weeks! And now the reason for the title of this post:
MY “Longest Ever” Ride
(at least in terms of the time spent away from home after leaving on a ride!)
On Wednesday, 23 May 2018 I set out on a training ride and didn’t return home until Wednesday, 30 May 2018, which was seven days longer than planned! And my ElliptiGO beat me home by those seven days!!
The ride was planned to be 41 miles, in a counter-clockwise loop that included Parbold Hill and then, in Horwich, Brazley Hill. I was experimenting with the handlebar mount for my Garmin Virb camera, filming and adding commentary as I rode. If I could have found a straight, smooth and traffic free length of road, I would have practiced taking the camera from the mount to pan the scenery while riding.
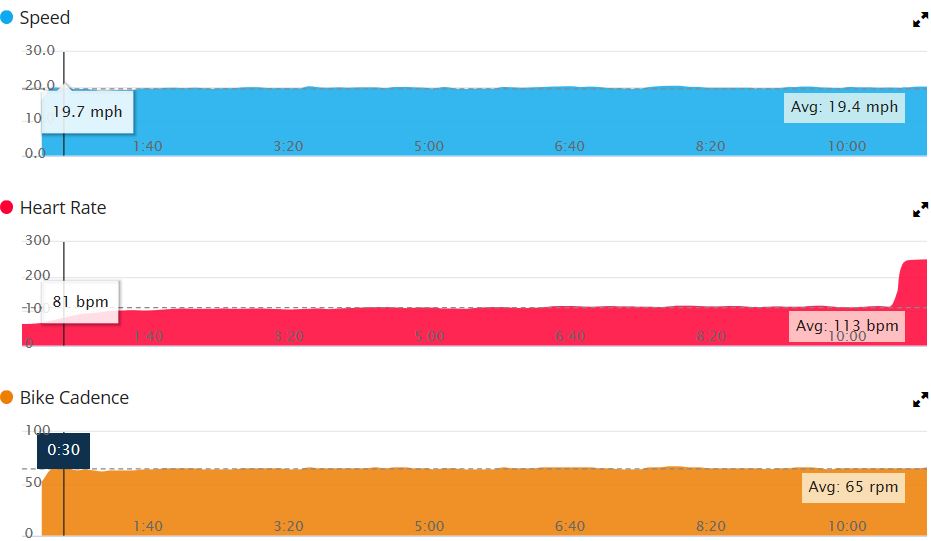
All was going well until I stopped to capture video of the view from the summit of Parbold Hill. The ride had been relaxed, despite a rogue couple of PRs (probably due to my improved fitness this year). The ascent of Parbold Hill drew, obviously, my maximum HR for the ride of 144 bpm and was completed slowly enough to allow me to breathe freely and remain unstressed (I’ve seen 159 on rides this year). Analysis of the ride and related data can be viewed here: The One I Didn’t Finish!
As mentioned earlier, I was experimenting with video during the ride. A compilation running to 5′.45″ of edited clips can be viewed here: Parbold Hill Ride. The conclusion of the video leads into the reason for me taking so long to get back home!
Background to an earlier experience
On 11 April 2018, I was riding my ElliptiGO, on a static trainer in the garage. I was spinning on the minimum resistance setting and barely 10 minutes into my warm-up as I slowly built towards the 21+ mph I was planning to hold for the remainder of the ride. Nothing changed by way of speed or cadence as I began to feel strange! My next glance at my Garmin raised alarm bells as I saw the unbelievable HR reading of 251 bpm! The combination of this shock sighting and me feeling peculiar conspired to make me feel more uncomfortable and did nothing to help my hypertension!

I tried to stay calm, stepped off the ElliptiGO, retrieved my Garmin from its bracket and returned indoors. Still not feeling quite right, but with no chest pain nor dizziness, I put it down to anxiety over the shock of what I thought was a Garmin glitch and rested to calm myself down while considering what action to take: ambulance – not warranted?; 111 (I thought they would be more qualified than me to decide whether an ambulance was warranted) – I called the number but the recorded message options were off-putting so, as I was now feeling better, checked my BP and HR (which were perfectly normal). Armed with this extra information, I called my doctors’ practise and was put through triage with one of the doctors before it was decided that nothing more need be done!
Picking up the story atop Parbold Hill
I had parked up my ElliptiGO and had removed my Garmin Virb from its cradle ready to walk around, taking in the cars in the lay-by, people on benches eating ice-cream, activity in the outdoor seating area of the pub and also the panorama on view from this vantage point. However, before I even started my walkabout, I began to feel uncomfortable. A glance at the Garmin revealed a 251 bpm HR – surely not a coincidence that once more a rogue Garmin reading followed a feeling of unease! Putting aside any video shooting, I went and sat on the pub wall to regain my composure then, when feeling up to it, re-parked my bike closer to the wall and moved to one of the trestle tables. I was now near to other people, hoping to soon be feeling normal again and determined that, at the earliest opportunity, I would demand a full medical review of what had happened to me. After several minutes, a full recovery seemed a long way off, the bright sunlight streamed through blurred vision and my Garmin was still showing 238 bpm. I asked a lady on an adjacent table if she wouldn’t mind calling an ambulance for me as I phoned my two sons, leaving messages when they didn’t answer.
It was a hive of activity as people then rallied to help. The lady returned with staff from the pub, having called the ambulance, and I was made comfortable, with my legs raised across two chairs. They even dragged over one of the table parasols so that I was in the shade as they made contact and liaised with my youngest son Chris. Upon arrival, the ambulance paramedic said that sometimes when HRs went into VT, fitness monitors spiked and gave inaccurately high readings. He could not obtain a pulse at the time but later confirmed that the Garmin reading was correct and that in all his time as a paramedic he had never seen a reading like it!
Despite feeling extremely unwell, I remained alert and remember being treated and at one time chewing on a rather large aspirin during the journey to A & E. On arrival, it was ‘all hands on deck’ as attempts were made to bring down my HR. A special drug had been administered for this purpose while electrode pads had been stuck to my chest in readiness should my heart need to be reset. My heart just wasn’t filling with blood. Before my HR had chance to revert, and before there was any chance to do a reset, I suddenly felt a severe nauseous wave and leaned to my left to vomit, which I don’t think I actually did! For, at that exact moment my heart stopped (according to the crash team). Next thing I remember was a sort of nudge and it was like a switch had been flicked as I immediately began to feel better. I had been shocked and I returned, with a normal HR, as quickly as I had gone!!
My time in the Coronary Care Unit
As I recovered in Resus, preparations were made for my transfer to the CCU and it was not long before my bed, with me in it, was transported through the hospital to the specialist ward. I was greeted, as I was wheeled through the doorway, by bed-one patient Ray, who introduced himself and the other two patients in the ward. During my stay there were seven people stayed in and left the ward. All but the latest two arrivals had been discharged from CCU by the time of my discharge. I met some diverse people with intriguing stories to tell and we had a great banter, not just among ourselves, but also with the cheerful staff who were also enthusiastic participants. Members of staff have even expressed an interest in seeing this blog post when it is completed!
Before I recount my recollections from my stay in the CCU, let me state that my care could not have been bettered. If Carlsberg did coronary care . . . then (to give it its full name) the Royal Albert Edward Infirmary coronary care unit would be their flagship . . . probably! The standard of care from all staff through several shift changes was so consistently high that it would be unfair to single out any examples. This in spite of the hospital, at the time, having to deal with industrial action, a bank holiday weekend and staff sickness. So, if you’re reading this, you know who you all are and how much you are appreciated. I love the Wigan dialect, although only a handful of miles from home, it has its own distinct charming nuances. Right CCU ladies and gents, here’s ‘your starter for 10’!! Who asked, “Is anyone available fo’ get a bag of saline?” Any names I do use in this account may have been changed to protect the innocent!!
What caused my cardiac arrest?
Following admission to the CCU, I had a chest x-ray and echocardiogram to supplement ongoing medication, bedside monitoring and frequent obs by the nursing staff. Then on Thursday 24 May 2018, the morning after admission, I underwent an angiogram through the radial artery in my right wrist. This was almost a carbon copy of the procedure I had in 2014, in that it was painless. Although again, when informed that, “During the next bit you will feel either a hot burning sensation, will feel nauseous or feel extremely uncomfortable – but it won’t last long!” (as I was infused), I did again feel extremely uncomfortable (like on my journey to A & E but more so). And, yes, it did pass very quickly. The procedure highlighted a severely narrowed left coronary artery, with lesions in the LAD and widespread disease elsewhere. Initial assessment pointed to a recommendation for a cardiac artery bypass graft, subject to review by the cardiology doctors.
Friday 25 May 2018, the morning after the procedure, I am bouncing! Feeling better than I have in a long while – even my arthritic knee appears to no longer bother me! Contrary to what is customary for me – to forget someone’s name within minutes of them being introduced – I had begun to remember multiple names. Pointing at a group of staff, I was able to rhyme off each of their names in turn. Remarkable! Was the electric shock I received some sort off elixir, will the effects be long-lasting? I am definitely in the right frame of mind to receive news of the next stage of my treatment.
After reviewing the Cardiac Catheterisation Report, together with its photos, the doctors were agreed that intervention via further angiography, angioplasty and stenting would not only be less intrusive and more readily available, but was likely to give just as good a result. So, it was back to the Cath Lab the following morning . . . I am on the Starship Enterprise. Captain James T Kirk is on the bridge, Bones and Spock hover over me while Scottie, Sulu and Uhura are at action stations! I’ve been informed that, as the left arterial route was being used, I would feel more discomfort than I did the previous day! After entering through the same radial artery, further investigation using Intro Vascular Ultra Sound, covered the atrium as well as arteries and branches, resulting in the discovery of scarring at the junction of a branch. This is believed to be the culprit for triggering the electrical rhythm problem. Upon being informed of this by one of the cardiologists, my mind went back to my caving / potholing days. Days spent squeezing through narrow passages with even narrower ‘occlusions’ caused by roof falls and then being rewarded by suddenly emerging into a vast cavern (atrium). My imagination wandered even more randomly – I’m with Raquel Welch in the microscopic submarine Proteus, on a Fantastic Voyage through blood vessels!!
I also had the strangest sensation, being aware of the catheter curving its way around my groin and down into my leg! This was accompanied by pressure on my shin, followed by what appeared to be kneading of my shin. As this wasn’t really happening, I can only assume that, as the catheter progressed on its journey it nudged against a nerve, referring the sensation down that nerve, and that the shin manipulation was nothing more than purchase of an elbow as the catheter was operated! – Or, maybe it was because Raquel Welch was sat next to me!! Unlike the previous day, and the angioplasty of 2014, I could feel every balloon inflation! It wasn’t painful but was a little unpleasant. The unpleasantness continued to a lesser degree as I recovered and the results of the internal trauma subsided.
Saturday 26 May 2018 and it is revealed that during that first night of recovery after my second procedure, a few seconds of Ventricular Tachycardia (VT) – of which I was totally unaware – were recorded telemetrically as I slept. This unwanted rhythm, thrown into the mix of the known coronary issues, then considered together with my ectopic rhythm and the other recent VT events, called for the re-introduction of a beta blocker as a first line of defence against future VT events. I had previously been taken off a beta blocker because, even at the lowest dosage, it lowered my already low resting HR into the 30s and, at times, caused light-headedness and anxiety. It was also suggested that it may be necessary for me to have an implantable cardioverter defibrillator (ICD) fitted. This device is capable of performing two roles: in the event of my HR becoming too slow, it would kick in like a pacemaker and speed up my HR to an acceptable level; or, on the off-chance of a VT event getting the better of the beta blocker, it would shock me to bring my heart back into a proper rhythm. Arrangements were made for me to have the procedure in Bolton the next Wednesday, conditional on consultation following further monitoring of my telemetry in the interim.
Overheard from a hospital bed in the dead of night
(or – why nurses are regarded as angels).
“John, you need to stay in your bed.”
“John, you need to stay in your bed.”
“John, you need to stay in your bed.”
“Yes, I’m staying in my bed.”
“John, you need to stay in your bed.”
“John, you need to stay in your bed.”
“John, what are you doing?”
“I’m going to the toilet!”
“John, you’re pulling your wires off!” “You need to get back into bed.”
“John, you need to stay here, in bed, while I bring you a bottle.”
“I don’t need a bottle.”
“John, do you not need the toilet?”
“Yes, I need the toilet.” “I don’t need a bottle.”
“OK John, I’ll bring you a bed pan but you need to stay in your bed while I get it.” “Will you stay in your bed for me?
“I won’t move.”
“JOHN, you’re going to pull out your drip – now get back into your bed and let me help you go to the toilet.”
“John, can you lift your bottom up so that I can put the bed pan under you.”
“John, you really need to sit properly on the bed pan.”
“You mean you want me to have a sh*t while lying down!”
and so it went on . . .
. . . until, after a period of quiet and with the patient now lying naked on his bed!
“Nurse – have you been tasked with monitoring my willy during the night!”
I wasn’t expecting to get any sleep that night – and I didn’t, but after “John” had become more lucid later in the day, I found out that he was 85 and had undergone a quadruple bypass. As I sat with other patients from the ward around ‘John’s’ bed we were fascinated to hear his life story. The nurse had used the bedside station computer, instead of the one in the office, to input data from her shift and stayed at this station, ensuring the wellbeing of her patient in need until the morning change-over. This certainly served to endorse and reinforce, in my eyes, the justified reputation of nurses as angels.
Sunday 27 May 2018 – Wednesday 30 May 2018:
Continual monitoring of my telemetry and stats sees me assessed as lesser of a risk and my priority place for the procedure is taken by a more urgent case. Wednesday morning 30 May 2018 and a second cardiologist is on the ward rounds and asks me to walk around the ward while he continues his rounds. I do lap after lap, figures of eight, reverse figures of eight and reverse laps but, when I stop to talk to one of the other patients on the ward, I am chastised with, “Walk! Walk!!” Later that afternoon I am visited by a third cardiologist. I am now considered such a low-level risk and it is borderline as to whether an ICD can be justified as necessary. The ball is placed in my court and, as I have a choice, I decide that I would like to have one fitted if it is still an option. I am told that, as I have a strong heart, this sways the argument in my favour. I can go home once my discharge papers are signed off and I will be now be attending for the Wednesday procedure as an outpatient.
Back Home
My first task, after my wife Margaret had brought me home was to organise my medication! I was due to reorder my next two month’s supply as I only had six days supply left. However, this usually routine process turned out to be quite a logistical challenge! At my discharge I was given a months supply of medication, which didn’t cover the whole range of my prescription so I had to plan my repeat prescription request accordingly. The on-line service was down Wednesday evening and Thursday morning so had to call the surgery! I waited to pick up my order from the chemist until Monday 4 June 2018, by which time I felt up to walking with Margaret the half mile each way. Also on the Monday I was called by Wigan Infirmary to check my availability, not to go to Bolton for my procedure, but to go to Wigan Thomas Linaker centre for a pre-op on Wednesday 6 June 2018 with the procedure now to take place in Bolton the following Wednesday 13 June 2018.
The pre-op appointment was just a routine check to establish that I was still suitably prepared for the procedure – no infection picked up in hospital or since, pulse, blood pressure / quality OK and a check that I was fully aware of what to expect of the procedure and of the ICD. On Friday 8 June 2018 the Royal Bolton Hospital phoned to confirm my appointment with written confirmation arriving the following day. Between my discharge from Wigan and my arrival in Bolton for the ICD insertion procedure I have filled in my spare time recollecting and recounting my experiences in this blog, which brings me to this point!
7:40 am Wednesday 13 June 2018
Margaret has conveyed me to car park next to the main entrance of Royal Bolton Hospital and we have made our way to the Coronary Care wards. A shift change-over is taking place, so we wait a short time for the oncoming team to organise my set-up in the coronary pacing unit. As in Wigan, the staff are all bubbly and cheerful as well as efficient, maintaining the positive experience I am having of the present day NHS. The NHS may have its faults but those faults certainly don’t lie ‘at the coal face’. The cardiac specialist arrives, introduces himself to Margaret and appraises her and me of the reason for the ICD, what it is able to do, about the procedure and what will happen post procedure. I walk unaided and climb up onto a bed in the cath lab.
I am soon swarmed by a well-honed team who festoon me with electrodes, wires, drip, protective cover, then sedate me and align me ready for the specialist to begin. Of course I am apprehensive as I don’t know what the next hour, or possibly longer, will feel like. However, I am assured that I am soon going to feel relaxed and that I should ask for more sedation if do feel any pain or discomfort. Well it wasn’t comfortable! But it wasn’t too uncomfortable and it certainly wasn’t painful as I felt myself and the plastic protection sheet being pushed about. I managed to relax and it didn’t seem long before it was all over – just one hour.
My bed was brought in, I was slid across onto it on a board then taken back to the cath lab side ward to be reunited with Margaret for refreshments and recovery. There was a swelling around my implant and it was standing proud, which prompted staff to apply pressure and see if they could disperse the swelling without having to resort to a pressure dressing. The specialist also called in to lend his weight and manipulation to return the implant to its desired position. In the next bed, the patient next in line for an ICD had been telling us that he grew his own grapes, and banter had then moved on, with the staff being offered / offering to tread / crush his grapes! If they had have already become proficient at this, they may also have been able to perform a Thai massage around my wound! As it was, I was given a compression dressing to keep the internal bleeding stemmed!!

Following the procedure, modelling the latest in compression dressings! Medication to stop blood clotting in my stents also allows blood to pool around wounds!

Blood pooling halted and dressing removed (along with body hair!) Good to go home, heal and hopefully for the swelling and scar to recede.
Job done! I was set free, allowed to go home to monitor my own initial progress as the wound heals. I was supplied with contact numbers and strict instructions to phone if I noticed anything unexpected. Although I was more than likely never to need its intervention, in the words of the specialist, I now have my own personal, portable paramedic.
Thursday, 14 June 2018.
I’ve had a reasonable night with plenty of sleep and the swelling has not returned. It’s now just a case of waiting for the excess glue to fall off the wound – I will be able to get it wet tomorrow. I’m limited in what I am able to do with my left arm at present and I’m not to lift it above my shoulder. So, what does the future hold? In four weeks time I will be free to drive again, provided the ICD does not shock me, in which case it will be six months. I will also be able to rehab my arm and shoulder back to full mobility. I will also be able to return to life as it was before I went into hospital. That means that I will be back on the ElliptiGO. However, in order to avoid keep putting my family through more worry, or even putting my ICD through its paces, I will be staying clear of long solo rides and long ascents! I’m taking the view of, “Been there, done that, got the tee-shirt!” And, as I did that only in the last year, I am going to wear that tee shirt with pride. I will be required to undergo medical checkups as will my ICD which will need to be replaced when its battery runs low (after 4 – 6 years).
I cannot praise the NHS highly enough for being there for me and for being able to draw on technology and expertise wrapped in a care system that is the envy of the rest of the world. Yes, definitely worthy of a Trip Adviser 5 star review!!
So there you have it – the story of my longest ride and its follow-up. Now that I’ve told my story I’d like to return to the reason why I have told it. Please look at the links below and if they motivate/inspire you to complete a milestone in your own life then don’t hesitate – go for it!
~o0o~

I think it’s time to ease off a bit now Tom. Hope you’re on the road to recovery 😊
LikeLiked by 1 person
That’s the plan. Don’t want to encourage the ICD to shock me!!
LikeLike